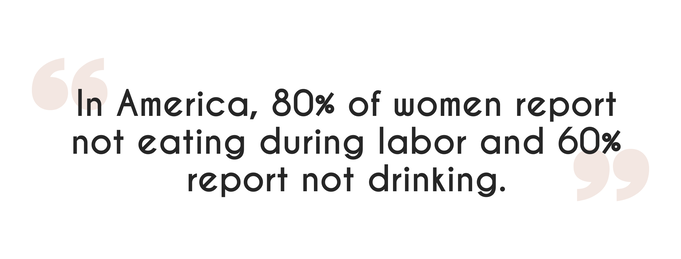
Labor is called labor for a reason. It is hard work. Not necessarily work that you have to put in as it happens involuntarily, but your body and the wondrous organ that is the uterus is working really hard during labor to get the baby in the right position and to push it out of your body. Hard work requires energy and that is where food and drink comes in! Have you ever wondered why many hospitals do not allow eating or drinking during labor? This overwhelming trend in hospital “policy” is for fear of aspiration (throwing up and choking on it) if general anesthesia (getting “knocked-out” and intubated) is needed. This started in the 1940’s when the drugs and tools used while providing anesthesia were very different. Luckily the field of anesthesia has drastically improved, making the probability of aspiration extremely rare. Some hospitals are heeding the newer research and changing their policies for low-risk pregnancies.
Many women feel that they could use a little nourishment, especially during long labors. Some women report no desire to eat during labor, especially as it intensifies. In quick labors there may not be time for it. Your body. Your taste. Your choice. If it is early labor, by all means, eat a well-rounded, nutritious meal until satisfied. Heavy meals are sometimes later regretted. Here are some food ideas that I have found laboring people like:
If you ate during labor, what were your foods of choice? When is a pregnancy no longer low-risk and fasting is recommended? Planned c-section. There are also some other potential factors that might increase your chances of aspiration such as: airway issues, eclampsia, pre-eclampsia, obesity, or opioids in your IV, but they haven’t been thoroughly studied. An epidural does not take you out of the low-risk category, but waiting a while after it is placed to make sure it doesn’t cause nausea is advised. Compare the eating policies at the local hospitals by downloading the Nashville Birthplace Comparison Guide. Sources // Evidence Based Birth
0 Comments
 Continuous, wired monitoring Image via Instagram: @thefirsthello Continuous, wired monitoring Image via Instagram: @thefirsthello Being mobile is key to managing pain during labor. Upright and mobile positions are associated with shorter labors, decreased pain, and higher overall satisfaction for mothers. Women often report that when laboring unmedicated, being confined to a bed is least favorable for coping, though when there is an opportunity to rest or sleep it's usually a good idea to take it! Pain management is largely affected by mobility, and mobility is affected by the cords around you, such as fetal monitoring of heartbeat and IV fluids. Thankfully, you have options for both! Monitoring: Continuous vs. Intermittent First, let’s talk about the two major types of monitoring: continuous (all the time) and intermittent (periodic, in intervals such as every 15-30 min). You may be asking yourself, is continuous monitoring actually needed? Research shows and ACOG agrees that for low-risk pregnancies, continuous monitoring is usually unnecessary and can actually create situations where more interventions are performed when not necessarily needed. Continuous monitoring is recommended for 1) inductions, 2) when an epidural is used, and 3) for some specific health conditions. So, if you are receiving medication, the risk for complications is higher, and additional monitoring is needed. Continuous In continuous monitoring, electronic fetal heart rate monitors are used to measure two things: 1) baby’s heart rate 2) contractions There are two devices that do continuous electronic fetal monitoring, and they both provide a digital display and print out of both the contraction and baby heart rate. The most common option and especially the one used during epidurals, uses two sensors that are wrapped around your abdomen and attached by a cord to a recording machine and monitor. As you can imagine, this requires you to be in or around the bed and near the machine. A newer option that many hospitals are beginning to offer for continuous monitoring measures the same two things, but uses bluetooth to send the signals, instead of cords. The sensors are attached as patches on the abdomen. This obviously allows for more mobility, which is a goal, but keep in mind that it also continuously monitors which is not the research-based recommendation for low-risk pregnancies with unmedicated labor. Cons to the bluetooth monitoring device:
The handheld doppler is used to listen to the baby’s heartbeat. You have likely used this device during your pregnancy at prenatal appointments with your provider when they listen for the baby’s heartbeat. The handheld doppler provides the opportunity for the most mobility during labor and can therefore, indirectly, be a great way to increase comfort level and manage pain. The device is portable, so it can go anywhere your nurse can go and you can be in nearly any position for them to get a reading.This device is waterproof and can even be used in the tub. It does require some additional training on part of the nurse, so be sure to ask your provider and hospital if nurses are trained and ready to use the handheld doppler for intermittent monitoring. IV During Labor IV's can largely affect your mobility during labor. When you have an IV, the pole must trail behind you which can be an annoyance during labor. Many laboring women report that they feel restricted by it, while others don’t notice it as much. The choice is yours! Typically, IV fluids are not needed in an unmedicated, low-risk pregnancy, BUT hydration and urinating are very important. Another Option To Consider Some hospitals also offer the option of a hep-lock or saline. This is a port where the IV catheter is inserted into one of your veins. It serves as an easy access port to your body for IV fluids or medications. When not in use, it can be taped off! Some families choose this option as a comforting precaution in case of an emergency since it is one less thing a nurse might have to do urgently. Other low risk women choose to forgo this option all together. Do you know which monitoring options are available at your chosen birth place? Download my Nashville Birthplace Comparison Guide to see your options. This guide compares each of these providers: Vanderbilt, St. Thomas Midtown, St. Thomas Birth Center, Baby + Company, Williamson, and Centennial. Here are some ways to be mobile and upright during labor:
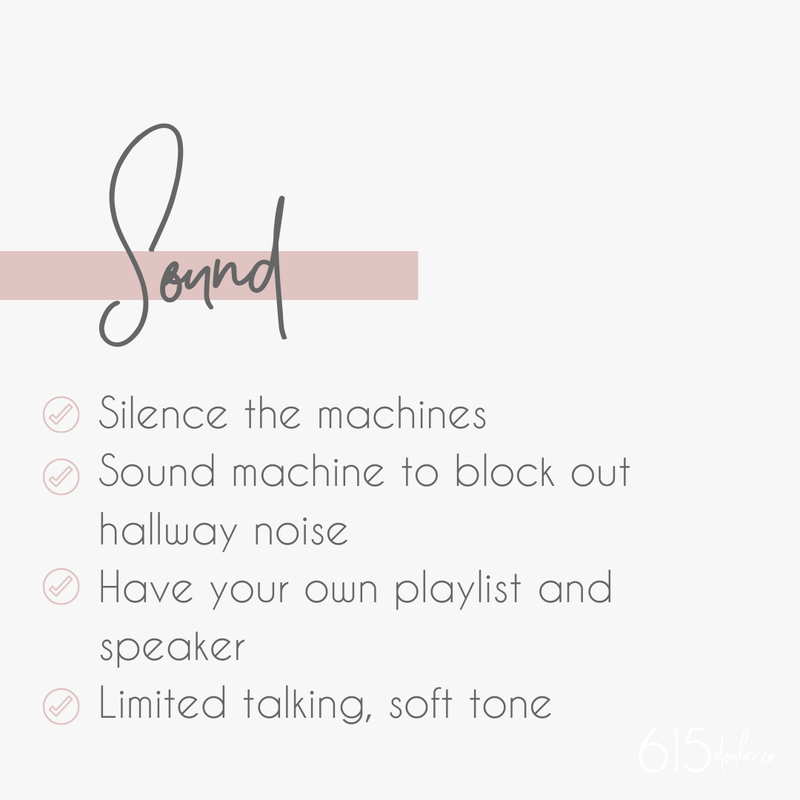
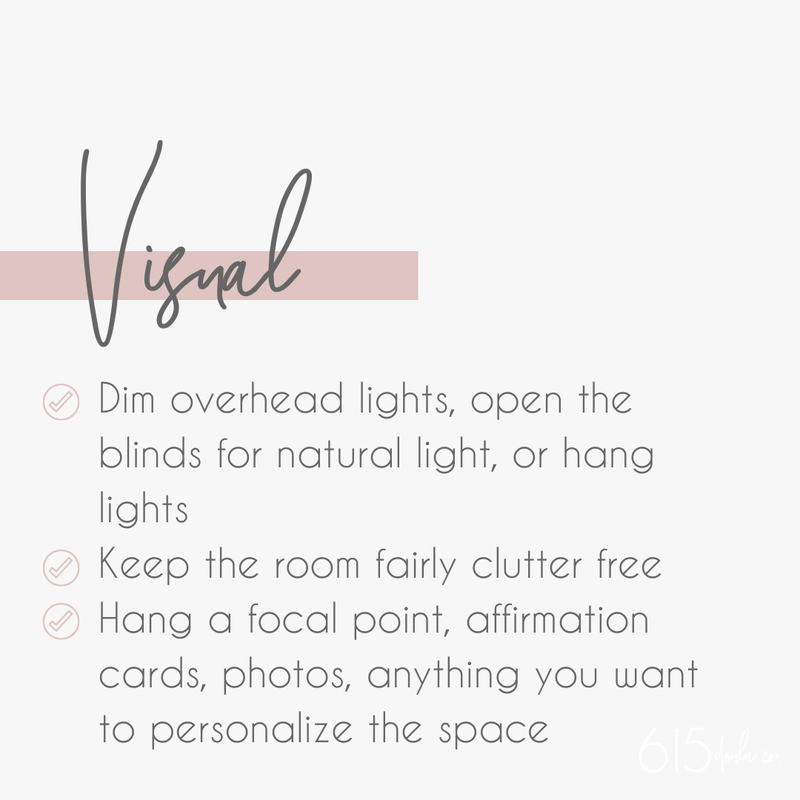
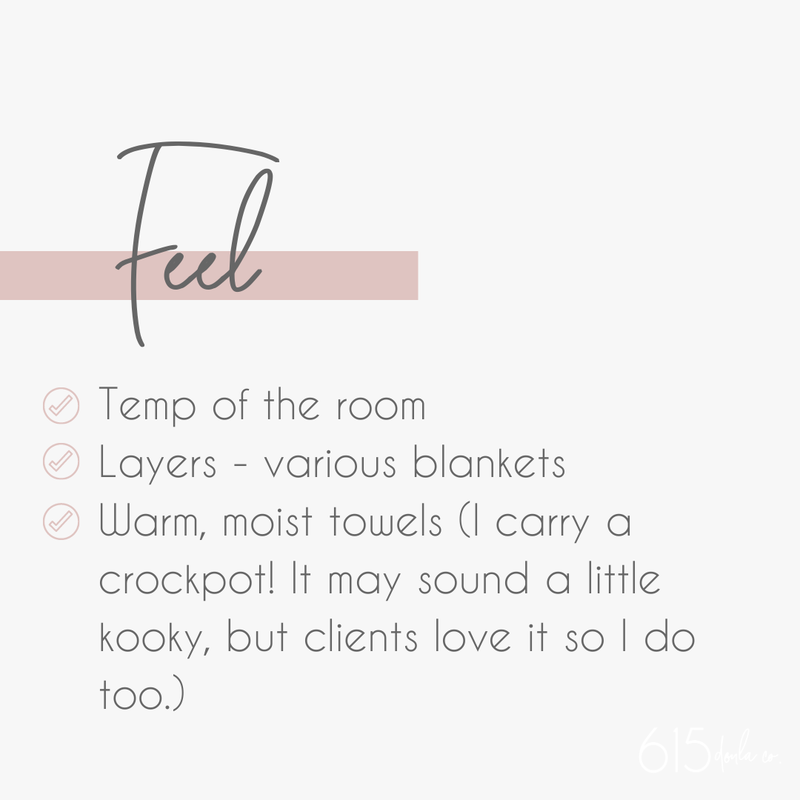
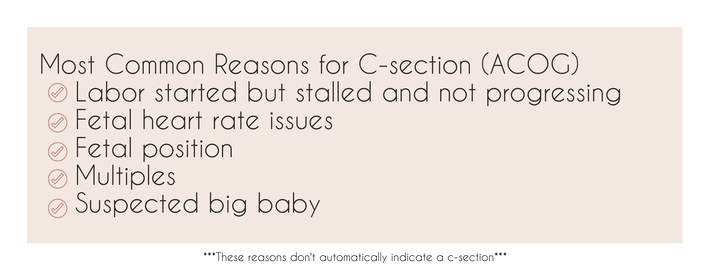
The 615 Doula Co Approach When I am supporting families in this decision, we will discuss your risk level along with any other determining factors such as if you are planning for a medicated or unmedicated labor. Regardless, hydration (and urinating) is key! I will be right beside you offering water continuously… One less thing you have to worry about! Sources // Evidence Based Birth  Image via Instagram: @mintandcocoaphoto Image via Instagram: @mintandcocoaphoto The environment of your birth space truly sets the tone for your birthing experience. First, you should ask yourself, how do I want to feel during birth? Do you want the vibe to be spa-like or a more energetic celebration? There is not a wrong answer to this question. It is totally dependent on your personal preference! Research shows that “Creating an environment that helps women to feel safe and secure during birth can improve women's experiences and likelihood of normal birth.” (Royal College of Midwives, 2014). A “private, undisturbed and dark environment, where women feel calm and safe can promote the release of oxytocin, the hormone responsible for uterine contractions and thought to promote the release of the pain relieving hormones endorphins” (Uvnas Moberg, 2003). When this environment is “not achieved, women can experience fear-tension-pain syndrome, impending labour progress and causing increased levels of pain” (Dick-Read, 2013). Here are some tips for creating a calm, spa-like environment in a hospital: During labor and birth, focus and composure are both very important. You may not think of things like beeping, talking, or a subtle hum of a machine as distracting until you are trying to coax a tiny human out of your body 🙂 The 615 Doula Co Approach Little things such as the vibe of your birthing environment might seem tiny in the overall birth plan, but trust me, these details are so significant in the moment. As your doula, I help walk you and/or your family through your birth space desires. We create a step-by-step plan on how we are going to achieve the vibe you want and uphold it in the actual labor space. Sources // Royal College of Midwives, Uvnas Moberg, Dick-Read, National Library of Medicine  First, let me be clear that there is NO ROOM for us to shame or guilt anyone about C-Sections. Birth is birth. However your baby enters the world, I’m here to support! Okay, let’s dive into the good stuff. What is a C-Section? A cesarean or c-section is a surgical delivery of a newborn through a series of 7 incisions through the abdomen and uterus. C-sections can be a life saving surgery and sometimes the safest delivery method, but for low-risk pregnancies, c-sections actually pose greater risks to maternal health and life. Most pregnant people rightfully want to avoid them. The US levels for c-section are currently too high (about 32% of all births). Did you know Doulas decrease the risk of cesarean by 39%? Pros
The 615 Doula Co Approach With all my clients, we sit down together and create a c-section plan in case that becomes the route for your baby to be born. Even with a c-section, you have options, and I am here to help you understand those options and feel confident in the plan that we’ve established. Sources // CDC, Evidence Based Birth, ACOG |
Meet Nicki
Hi, I'm Nicki! I am a Nashville based Doula and founder of 615 Doula Co! My favorite part of working as a Doula is supporting families through the life transitions of pregnancy, birth, and postpartum life. Explore Blog |