|
Fetal monitoring is a birth preference that can have a significant impact on how you labor, so digging into the info to see what aligns with your preferences and needs is worthwhile. There are so many options when it comes to monitoring baby in utero, from intermittent monitoring to continuous monitoring and all the different machines to do so. Here at 615 Doula Co., education and having information before you need it is one of our top priorities. This blog post breaks down:
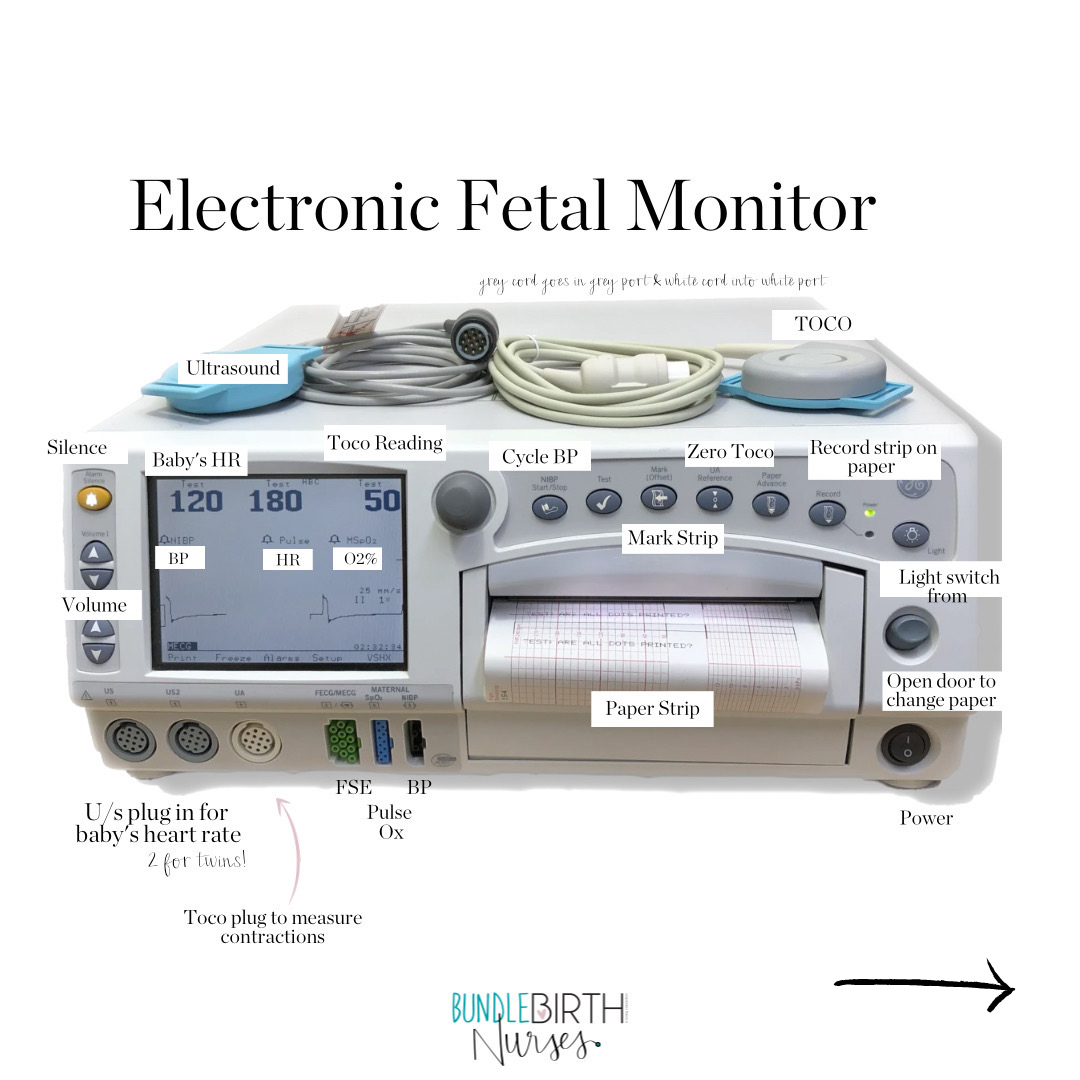
Let's get to it! What is Fetal Monitoring?Fetal Monitoring is the act of using various types of instruments to help monitor baby during labor. What Does Fetal Monitoring Measure?There are four different metrics throughout labor. Not all tools/machines measure each one, but the four possibilities include: 1. Baby’s Heart Rate: This is the main form of fetal monitoring, regardless of the type of monitor used (we will get into that later). It tells us how baby is handling labor. The average fetal heart rate during labor is in the range between 110-160 beats per minute. Baby’s heart rate may vary by 5 to 25 beats per minute as baby responds to labor. 2. Variability Pattern: When monitoring the heart rate pattern, some accels (peaks) and some decels (valleys) are normal and this variability is a good sign. These accels and decels show baby is responding to contractions. However, persistently low dips can call for some changes during labor (i.e. positions changes, hydration like IV fluids, and further intervention if those don’t work). 3. Contractions: Some forms of monitoring also track pressure, i.e. contractions. When evaluating baby’s heart rate, knowing when the accels and decels are happening before/during/after contractions gives additional information to how baby is doing. If utilizing an epidural, some epidurals cover the contraction sensation, so tracking contractions can be helpful in navigating your labor. 4. Maternal Heart Rate: Some forms of monitoring also track your heart rate. This can be useful, especially if the fetal monitor begins picking up on your heart rate (we don’t want that confusion because our heart rates are much lower than a baby’s). A persistently high heart rate might be a sign of a developing infection. The Two Main Types of Monitoring: Continuous vs. IntermittentWhen thinking about how you want to labor, one important choice to consider is what type of fetal monitor you prefer. Before choosing what type or tool you want used for monitoring, you first want to decide your preferences and needs for intermittent vs. continuous monitoring. As the words suggest, continuous monitoring is continuous, without breaks during labor. Intermittent monitoring checks in on baby at set intervals during labor (commonly every 30 or 15 minutes depending on the stage of labor). Continuous types of monitors (i.e. the Electronic Fetal Monitor, the Bluetooth Monica, etc.) and Intermittent types of monitors (a handheld doppler) both have pros and cons in their usage. Below, we lay out some pros and cons. Huge shoutout to Evidence Based Birth for being the brains behind these pros and cons. Check out their website here; they have amazing resources for all things birth. Continuous MonitoringPros:
Cons:
Intermittent MonitoringPros: -Lower rate of cesareans, vacuum, and forceps -Supports mobility and position changes (key for coping through unmedicated labor) -Can be used in shower or tub -Leads to more continuous, hands-on support from providers during birth Cons: -Higher rates of newborn seizures, though still rare regardless at .2% -May not be appropriate for some high-risk pregnancies or those with complications -Staff must be trained on how to log data instead of relying on machine that does it for them -Requires 1:1 nurse to patient ratio to provide this hands-on care Note: If your risk level changes during labor, your type of monitoring preferences may need to pivot. Types of Fetal Monitors Image Credit: @emanating_kate on Instagram Image Credit: @emanating_kate on Instagram 1. Intermittent Doppler with Handheld Ausculation Pros:
 Image Credit: @midwifeco.dfw on Instagram Image Credit: @midwifeco.dfw on Instagram 2. Monica Novi Bluetooth Monitor Pros:
 Image Credit: gehealthcare.com Image Credit: gehealthcare.com 3. Portable Mini Telemetry Unit Pros:
 Image Credit: @heartsandarrowphotography on Instagram Image Credit: @heartsandarrowphotography on Instagram 4. Electronic Fetal Monitor This is the most commonly used monitor in the US. It is often the default option. Keep reading until the end to learn more about how to read the data this puts out. Pros:
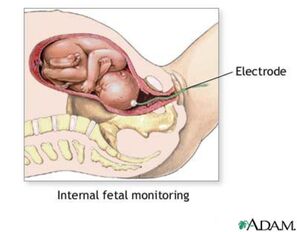 Image Credit: Google Images Image Credit: Google Images 5. Fetal Scalp Electrode for Internal Monitoring Pros:
You Get to ChooseFetal Monitoring is a birth preference. Of course, your preference may need to change or be shifted if your risk level changes during labor. However, always remember you do have a choice and knowing your options before birth helps to ease the mental load if you have any turns in the road during labor.
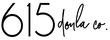
Demystifying the Electronic Fetal MonitorIf you are planning to give birth in a hospital, this info on the electronic fetal monitor is important for you to understand what is going on in the labor room. The Electronic Fetal Monitor is most hospital’s default option and is therefore used in most hospital births. If you are planning for an unmedicated birth, you will likely want to choose another monitoring option, but having this basic knowledge in case of any pivots in labor, can be helpful. This monitor is also often used in triage, regardless of your preferences for medicated/unmedicated. If you are planning for an epidural or induction your chances of using this machine are much higher. Here is some basic info to demystify it. If you are planning on using the Electronic Fetal Monitor
Don’t forget, continuous monitoring is not evidence-based for low-risk labors that are unmedicated. If you do want/need continuous monitoring, you have other tool options. A special thanks to Bundle Birth Nurses for these labeled images. You can check them out at https://bundlebirthnurses.com/ or on Instagram @bundlebirthnurses. Next Steps
0 Comments
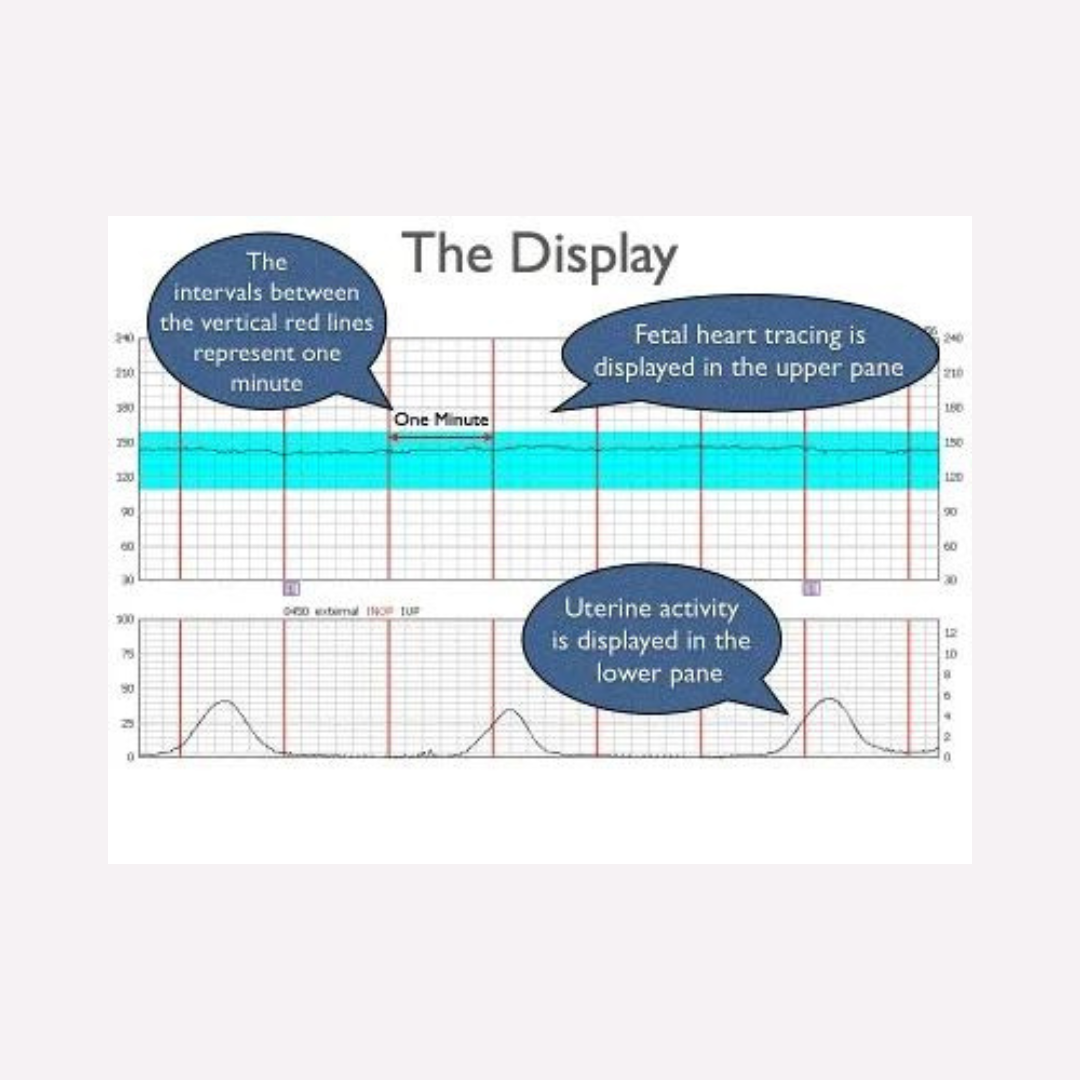
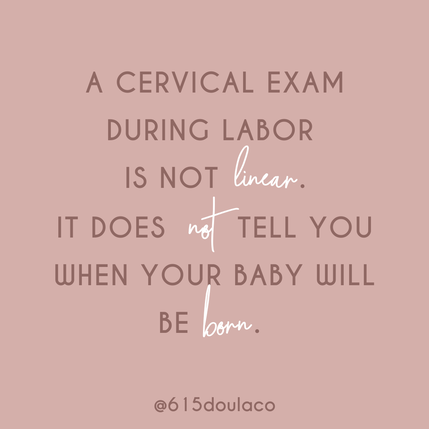
What do you know about your cervix? We find that many of us aren’t well informed about our cervixes, but it is such a dynamic and interesting part of our body and does so much during our fertility, pregnancy, and birth journeys. So, we have compiled a blog post to give you the 411 on your cervix! This comes after our Instagram series on the cervix in honor of January’s Cervical Health Month. Let's start with the basics...What is a cervix?The cervix is a canal that connects your uterus to your vagina. It comes from the Latin word ‘neck’ and is sometimes called the "neck of the uterus". In the below image, you can see that the cervix in a non-pregnant woman, tilts more towards the back. Some Interesting Facts about the Cervix:
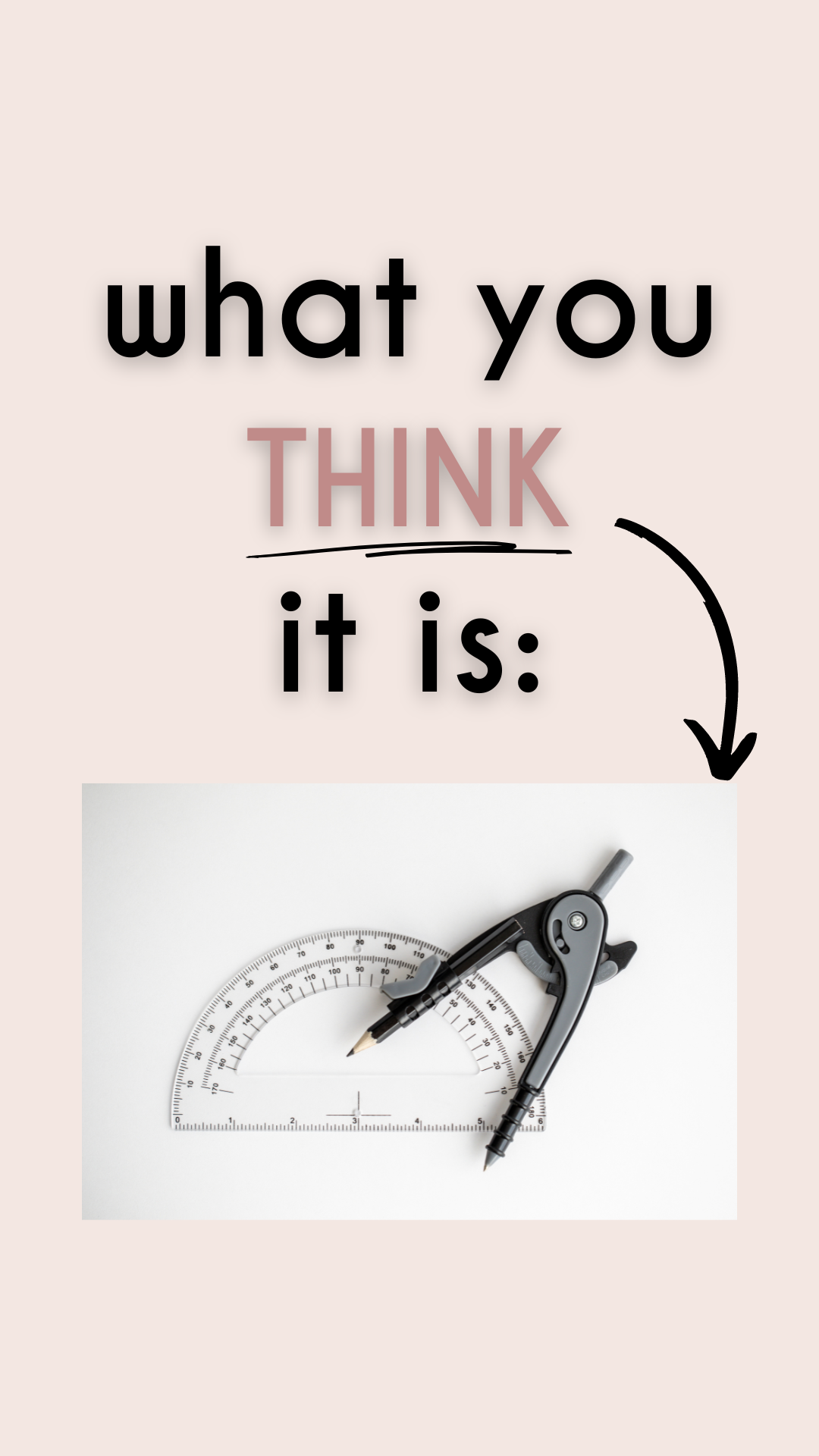
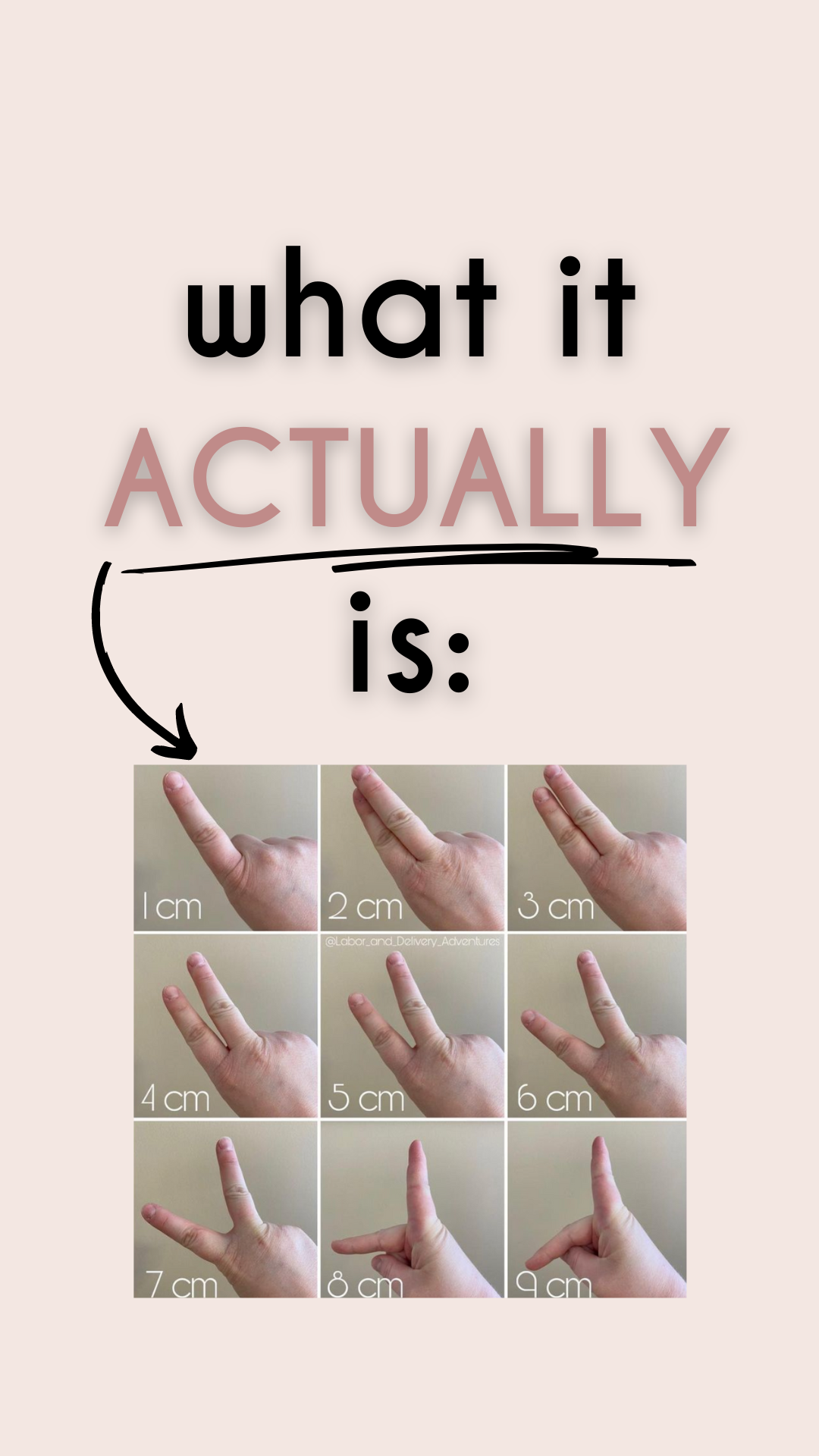
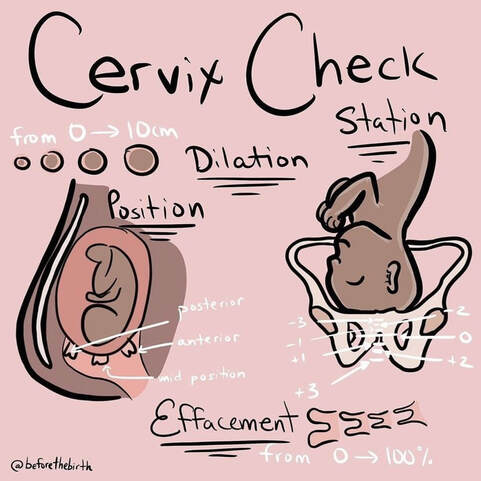
Now that we have labeled, and chatted about the non-pregnant cervix, let’s move into talking about the cervix during pregnancy. We will discuss: what a cervical exam is and what it is not, what cervical checks measure, pros and cons of cervical checks, and how to advocate regarding cervical checks during pregnancy and labor. What is a Cervical Exam (or cervical check)?Cervical exams check the cervix for common changes that occur throughout pregnancy and labor! You may think that measuring a cervix is a precise business that includes a special tool. It's not! It is literally someone spacing out their fingers to determine how many centimeters open the cervix is. As you can imagine, this is highly subjective. Many labor care teams work to norm their measurements, but we commonly see one provider like an OB saying one dilation and then a nurse or another care provider saying another. It can really throw you for a loop, but as long as you know, you can temper your expectations of its precision. What Does a Cervical Check Measure?Well first, they measure more than just dilation! They actually measure 5 different metrics:
Pros and Cons of Cervical Checks During LaborAs with many things during birth, there are pros and cons. We believe it is very important to be informed and to know both the positives and negatives of birth options. This stands true for cervical checks as well. Below are *some* of the positives and negatives of cervical checks during labor. Once you know some of these positives and negatives, you can make an informed decision about them for your birth plan and then advocate for your preferences during labor. Pros: - gives data that can be helpful, such as whether to be admitted to your birth place. As a doula trained in spinning babies, it gives me some additional data points to recommend specific positions or movements to ensure baby is in the best position for a smooth birth. - can encourage you if you like the way you are progressing - can give you the go-ahead to push with the urge after 10 cm (we don't want to push before 10 - the cervix can swell) Cons: - introduces bacteria and therefore increases risk of infection - it can hurt and feel foreign - can disrupt your labor flow, including getting in an uncomfortable position - can discourage you if you haven't yet made the progress you were hoping for - some may pressure you to begin pushing as soon as you reach 10cm, instead of honoring "laboring down" and spontaneous pushing (see previous posts re: pushing) A Note About Cervical Exams During PregnancyIncreasingly, routine cervical exams during pregnancy (without specific evidence of need) are going to the wayside, and for good reason. Sometimes you still hear that OB's are requiring cervical exams during pregnancy, sometimes early on, and for all of their patients. We also hear of OB's beginning/restarting cervical exams weekly at 36 weeks. Some offer it and others expect it. We find that there is a fairly reliable overlap with the doctors that do routine cervical checks during pregnancy and those that favor old-school hospital style birthing where they know better and intervene often (inductions, pushing on your back, limiting food and drink, etc.). We find that many of the most consent and evidence-based providers that honor the safest low-intervention path, don't usually have routine cervical exams as part of their pregnancy care protocol. It might not be the full picture of a provider, but it is a clue. As always, there are exceptions. For example: if you have a history or there are signs for preterm labor, a cervical exam could be helpful in mapping out your care plan. You, do you. You Get to Choose
Here are our best tips:
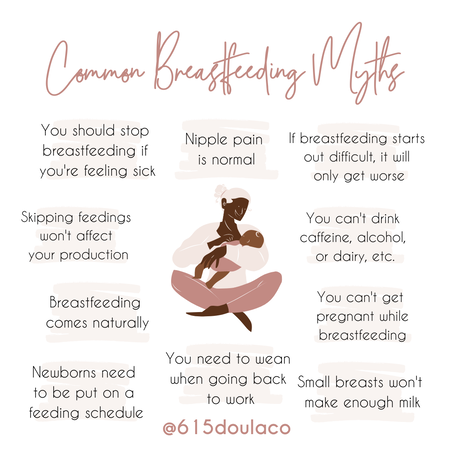
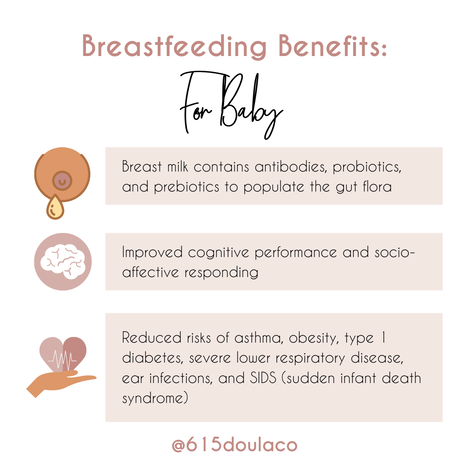
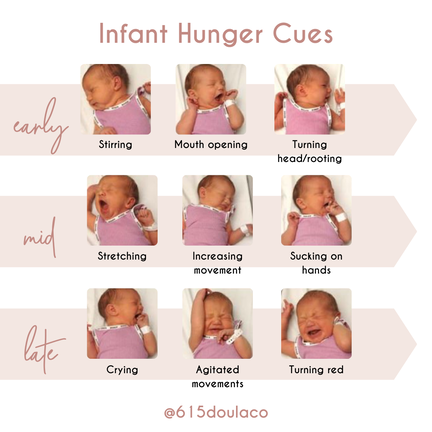
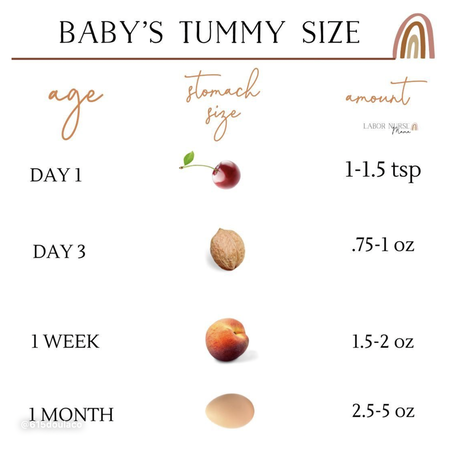
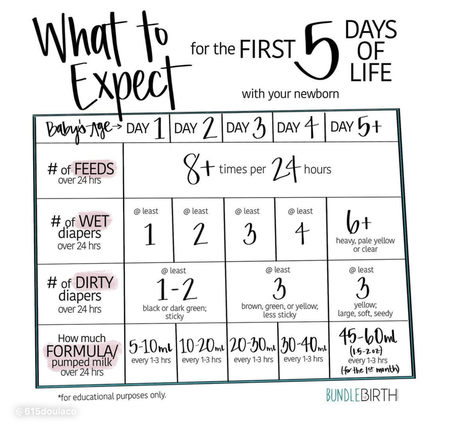
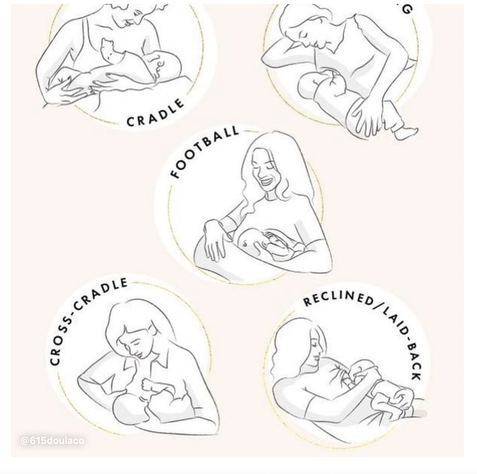
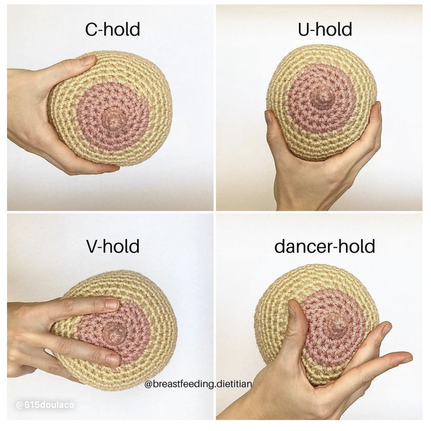
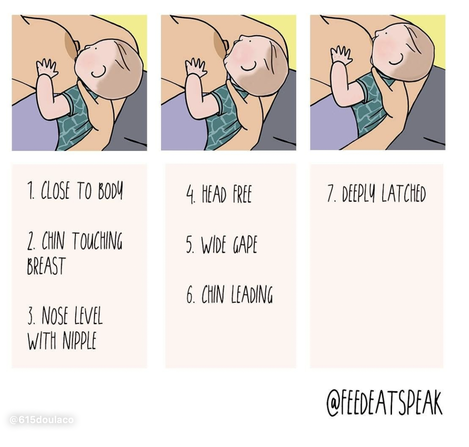
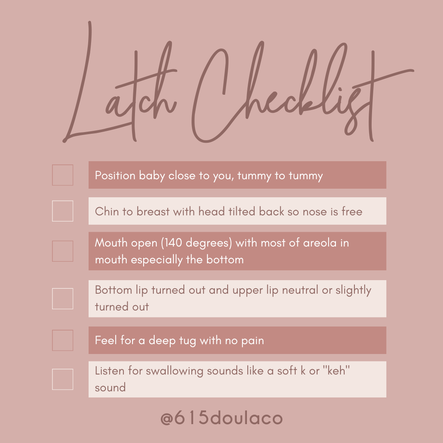
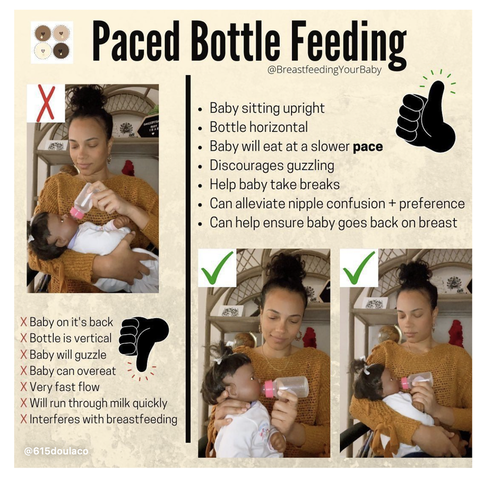
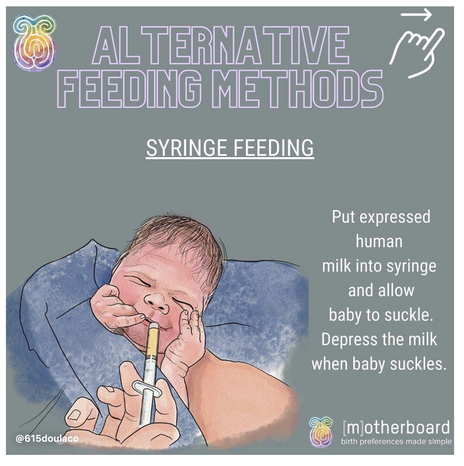
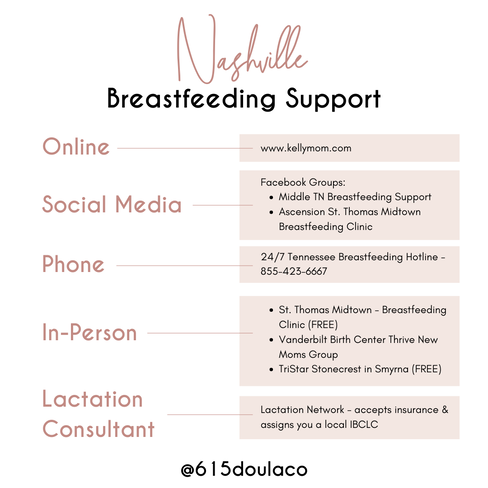
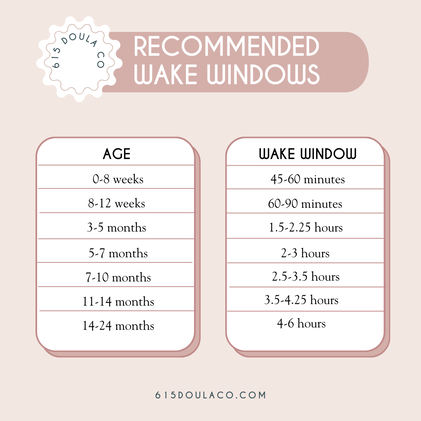
This blog is a collection of breastfeeding‑related posts that @615doulaco put together in honor of National Breastfeeding Month. What once used to live in Instagram Guides, now lives on the blog! Breastfeeding can be hard work, but with education and support, you and your baby can find your groove! Conversation StarterBreastfeeding Myths BustedWays Your Partner/Support People Can Help YouThe Benefits for Both You and BabyHow to Know When Baby is HungryWhat is Colostrum and How is it Good for BabyHow Much Colostrum or Milk Does a Baby Need?Save Your Sanity and Focus on the FactsHow Do I Know My Baby is Getting Enough Food?Breastfeeding Positions to TryBreastfeeding Positions ContinuedCommon Breast HoldsUnderstand How Baby LatchesQuick visual reminder for getting a strong latchLatch ChecklistGet a Deep Latch with the “Flipple” Technique“Flipple” IRL ExampleLearn How to Hand ExpressSome Thoughts on How Long to BreastfeedHow to Properly Store BreastmilkPaced Bottle Feeding ExplainedAlternative Feeding MethodsYou're Doing Great Mama!Local Breastfeeding SupportWake WindowsWaking Baby to Feed Are you pregnant in Nashville and wondering how to choose the right OBGYN or midwife for your pregnancy and birth? Here are some of our top tips. Choosing a quality midwife or OBGYN for your pregnancy is an important decision and is key to having a positive birth experience. Like many of the decisions in pregnancy, it can also feel overwhelming. You want to find someone who you feel comfortable with, someone you trust, and someone who you know will provide you with the best possible care. In our work with Nashville families, we have found this process to be helpful in choosing your provider: Ask Yourself:
Reach Out For The Intel:
Tour and Interview:
Don’t be afraid to Switch Providers during Pregnancy:
|
Meet Nicki
Hi, I'm Nicki! I am a Nashville based Doula and founder of 615 Doula Co! My favorite part of working as a Doula is supporting families through the life transitions of pregnancy, birth, and postpartum life. Explore Blog |